Guest blog post by Anatomy Trains Certified Teacher Dr. Meredith Stephens.
Editor’s note: Dr. Stephens will be teaching Understanding and Working with Osteoporosis as part of our 2021 Maine Summer Course program, July 23-24. She will also be teaching Understanding and Working with Scoliosis, July 25-26.
Trabecular Bone Score: What it is and why you should know it
If you have osteoporosis, you may be familiar with dual X-ray absorptiometry or DXA. This is the test that is most often done to diagnose osteoporosis. The DXA test generates a T-score that determines if your bone mass is normal, if you have low bone mass (aka osteopenia), or osteoporosis (see Figure A for how scores are interpreted). The information is used to help you and your physician decide on your treatment options, e.g. exercise, diet, and/or medications.
Figure A – T Scores generated by DXA testing for bone density:
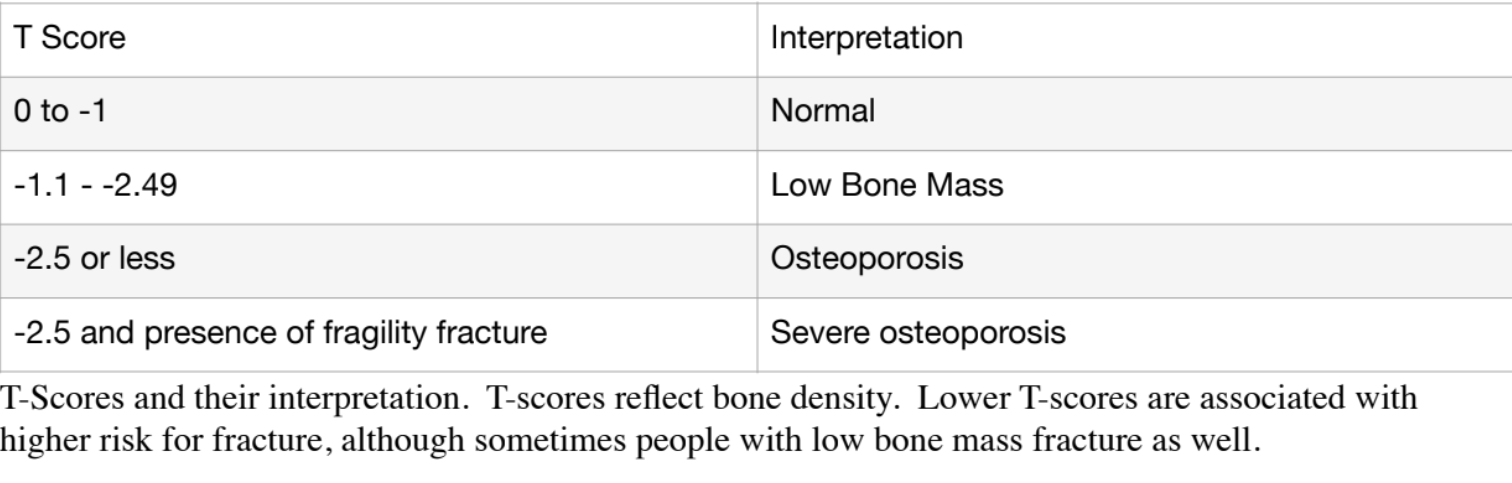
Historically, some women with osteoporosis never sustain a fracture, whereas others with only low bone mass do fracture. This highlights the incomplete picture given by the DXA test. The problem with DXA is that it only tells you your bone mass or density, not bone quality, which has been identified as the missing piece of the puzzle in terms of predicting fracture risk. (Now don’t get me wrong, there is plenty of statistical data to support the use of DXA in fracture risk assessment and the rationale for treatment!)
Although there has been much research into what constitutes bone quality and how to measure it, many of the new tests and measures are still in the research phase and not yet available. The good news is that one relatively new test, the trabecular bone score (TBS) is emerging as a tool to assess bone quality. While still not widely used, it may help in getting a more complete picture of your bone health.
What is Trabecular Bone Score (TBS)?
Trabecular Bone Score, or TBS, is a computer software application that is installed on DXA machines. The program takes the DXA image of the lumbar spine (low back) and creates a greyscale pixel image of the vertebral trabecular bone microstructure. The resulting image provides an indirect measure of the trabecular microarchitecture. A dense structure, with lots of well-connected trabeculae, has a large number of pixels with small amplitude changes. They are variations of very light and light grey. Think of it like a dense sponge with very small holes.
A porous structure has fewer pixels with much greater amplitude in their color variations. They are light where bone is present to very dark or black where the structure has broken down and appears more porous or full of holes. This is like a sponge with large holes or spaces.
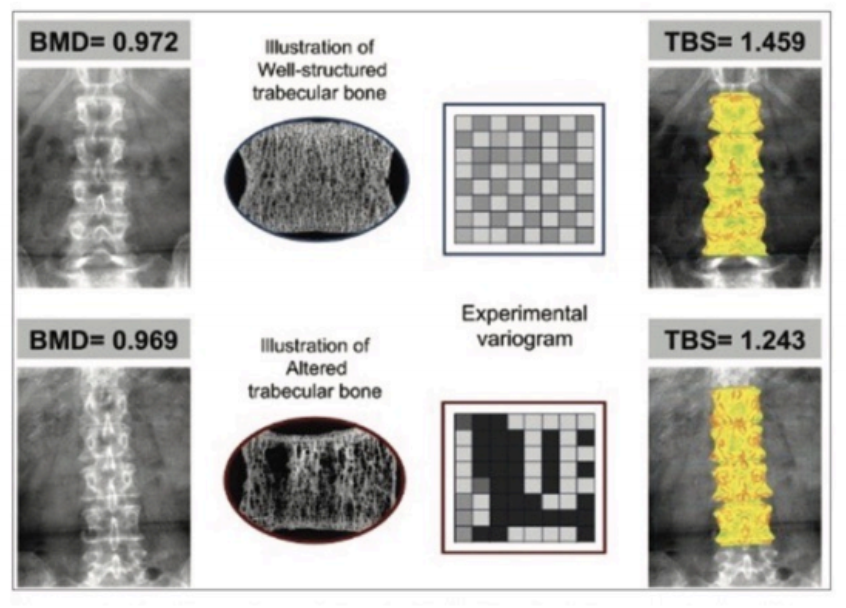
Source: Rajan et al. Indian Journal of Endocrinology and Metabolism. 2020; 24:237-243.
As illustrated above, even with similar age, BMD and BMI, the quality of the bone can be very different.
Trabecular bone score may be used in conjunction with the T-Score to determine if the microstructure is compromised in addition to the T- Score diagnosis of low bone mass or osteoporosis. Or conversely, if there is low bone mass or osteoporosis but good microstructure. This extra piece of information may help you and your doctor decide what the best course of treatment is for you.
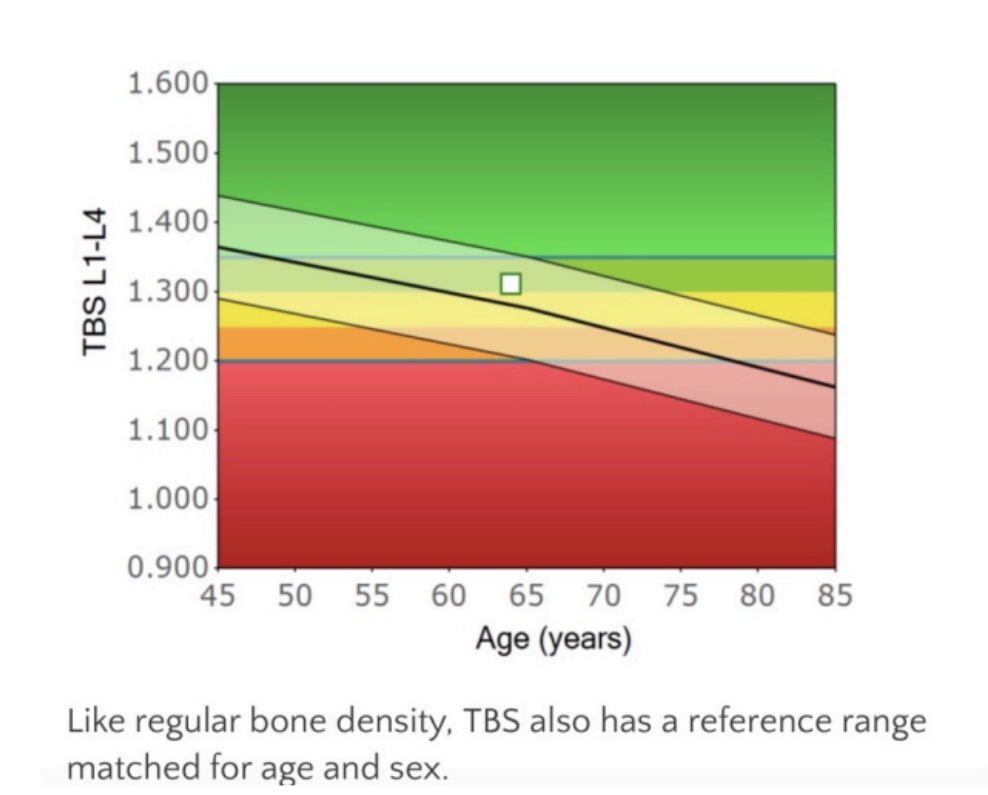
Below is the reference range for TBS. (Source: https://www.chatswooddensitometry.com.au/trabecular-bone-score-tbs.html for explanation. Full interpretation of reference range goes beyond the scope of this article.)
Although TBS has been studied and used for over 13 years, it is still not universally used or covered by insurance in the US. (americanbonehealth.org)
Here are some other pros and cons to TBS.
Pros
- It may be less affected by arthritic changes in the spine, which can artificially
increase BMD T-scores.¹ - May be used to indirectly determine bone micro-architecture. Some
researchers state that it is an independent predictor for fracture.⁴ - Helps in clinical decision making…now there is a measure of quantity (BMD)
and quality (TBS). - Shows promise as a fracture risk tool for those with secondary osteoporosis (such as hyperparathyroidism) whose bone structure may have been impacted. Also for those with Type II diabetes and glucocorticoid use.¹
- May be used in conjunction with BMD testing for monitoring anabolic therapy.³
- The combination of TBS and BMD scores may be better at predicting fracture than either score alone.⁴
Cons
- Since TBS is installed on and used with a specific DXA machine, you cannot take a previous test and have a TBS done. It must be done on a DXA that has the software.
- Some research indicates TBS may not significantly change FRAX score for fracture prediction for those with primary osteoporosis¹. However, other research supports its use to create a more nuanced risk level at any BMD (see web reference B).
- Score may be falsely increased by bony outgrowths between the vertebra of the spine (syndesmophytes).¹
- TBS is negatively correlated with increased soft tissue/BMI in the body. As soft tissue increases, TBS is underestimated. This may be due to a limitation of the algorithm.² Newer versions are being tested for improved accuracy.²
- May not be useful in assessing anti-resorptive therapy as BMD changes more quickly than bone micro-architecture.¹,³
- Scoring may vary with different DXA machines.³
More research is needed to determine clinical norms for TBS and what constitutes the least significant change over time (which may vary with each DXA manufacturer).³ Clinics need to be able to calibrate machines in the manner they do for DXA testing so you know that the results you get from test to test can be compared with confidence. But, the TBS does help get a more complete picture of your bone health.
Where can you get it? Medimaps is the maker of the TBS software. (**Remember TBS is not a stand-alone test. It is installed on the DXA machine and is calculated from the DXA test for that machine.) Refer to the link to Medimaps site (reference C in the web reference section) to help you find a location that includes TBS with the DXA test near you. You may consider getting your next test at a site that includes the TBS.
References:
1. Rajan R, Cherian, KE, Kapoor N, Paul, TV. Trabecular bone score—an emerging tool in the management of osteoporosis. Indian Journal of Endocrinology and Metabolism. 2020; 24:237-243.
2. Shevroja E, Aubry-Rozier B, Hans G, et al. Clinical performance of the updated trabecular bone score (TBS) algorithm, which accounts for the soft tissue thickness: the OstoLaus study. Journal of Bone and Mineral Research. 2019; 34(12): 2229-2237.
3. Krohn D, Schwartz EN, Chung YS, Lewiecki EM. Dual-energy x-ray absorptiometry monitoring with trabecular bone score: 2019 ISCD official position. International Society for Clinical Densitometry. Journal of Clinical Densitometry: Assessment & Management of Musculoskeletal Health. 2019; 22(4): 501-505.
4. Hans D, Goertzen AL, Krieg MA, Leslie WD. Bone microacrhitecture assessed by TBS predicts osteoporotic fractures independent of bone density: the Manitoba study. Journal of Bone and Mineral Research. 2011; 26(11): 2762-2769.
Web references:
A. This Australian site gives a nice visual representation of how the TBS can be
used clinically with BMD scores: https://www.chatswooddensitometry.com.au/uploads/6/3/8/4/63847651/interpretationguidlineshandoutlandscape.pdf
B. This site: American Bone Health. org has more information about TBS and a somewhat harder to interpret color chart that has a more nuanced risk level that combines TBS with BMD. https://americanbonehealth.org/bone-health/howtesting-bone-structure-helps-predict-broken-bones/
C. Medimaps and Finding a DXA with TBS location near you https://www.medimapsgroup.com/tbs-osteo/ https://www.medimapsgroup.com/find-a-clinic-with-tbs/